
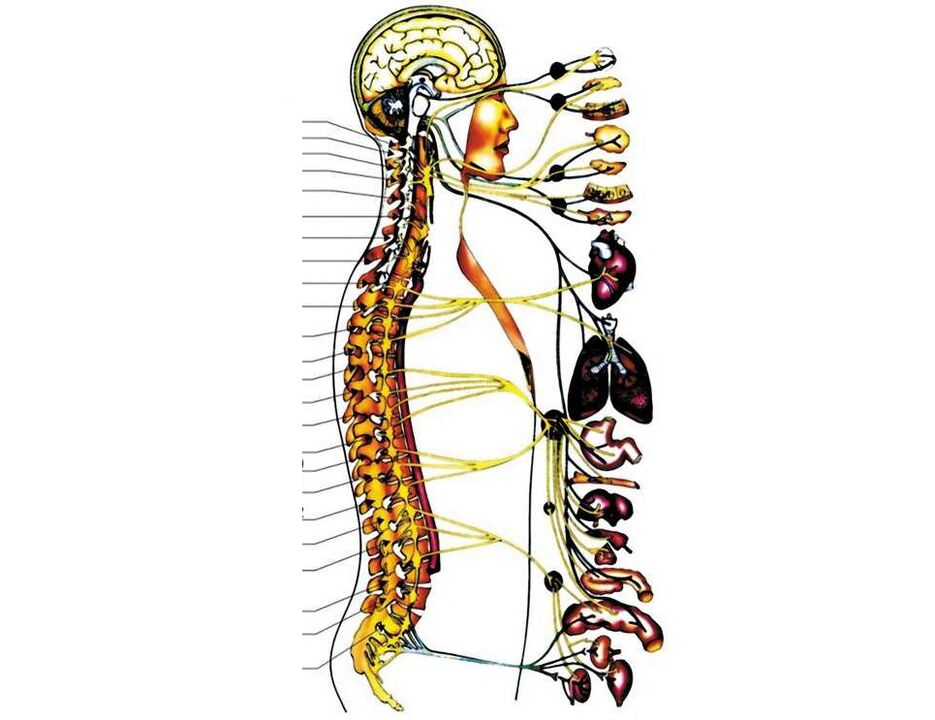
Osteochondrosis without treatment not only causes constant pain in the back or neck, a feeling of incomplete inspiration, or disruption of the heart. It is dangerous by squeezing the nerve roots, which can cause paralysis, impaired sensitivity, erectile function, and fecal and urinary incontinence. Developing in the cervical spine, osteochondrosis leads to a deterioration in the blood supply to the brain, which causes headaches, dizziness, and mental activity progressively worsens. In addition, changes that occur in one segment of the spine soon spread to other segments, and then to the entire spinal column.
In the article we will consider the types and classification (degrees, stages) of osteochondrosis. This will help a person with a similar diagnosis to better understand their current situation with the development of this disease and possible treatment.
Types and classifications of the disease
Osteochondrosis is a violation of nutrition, the removal of dead cells and their metabolic products (the so-called "slags") in the disc (a special shock-absorbing layer) between the vertebrae, as well as in the parts of the vertebral bodies adjacent to it from below and above.
What is osteochondrosis?
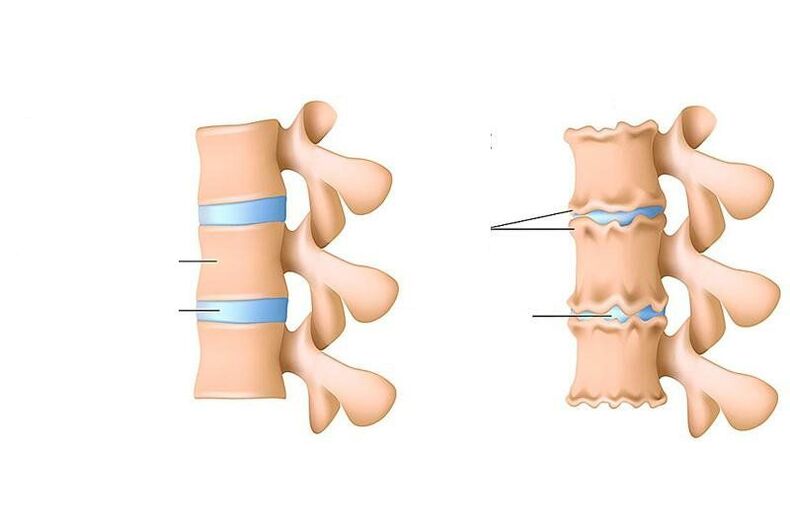
In adults, the diagnosis of "osteochondrosis" is understood only as the development of dystrophic (associated with malnutrition) processes in the cartilage of the spine. If, in adults, processes similar to osteochondrosis (thinning of the cartilaginous tissue lining one and the other bones of the joint, subsequent changes in the bones themselves) occur in one of the joints (for example, in the knee joint), this is called deforming osteoarthritis.
In adolescence (from 11 to 18 years old), the term "osteochondrosis" is applied not only to the spine. This process is called juvenile (youthful) osteochondrosis. When it develops in the spine, it is called Scheuermann's disease. But it can also have other localizations (for more details, see the corresponding section).
The classification of osteochondrosis takes into account:
- in which department malnutrition developed (classification by localization);
- how severely the intervertebral disc is affected (classification of osteochondrosis by periods);
- whether there is now acute inflammation or it subsides (domestic classification of grouping by stages).
Adults also have a separate type of osteochondrosis. This is Kienböck's disease in adults (osteochondrosis of the lunate bone, which is located among the bones of the wrist).
The diagnosis may also indicate that osteochondrosis is post-traumatic. This means that the beginning of the violation of the structure of the intervertebral disc, the hyaline plates located between the vertebral body and the disc, as well as the vertebral bodies themselves, was caused by trauma. The injury can be instantaneous and severe (for example, with a strong blow to the spine), but post-traumatic osteochondrosis can also develop as a result of a permanent injury of not very great strength (for example, constant tilts with weight in loaders or athletes who perform tilts, lifting the barbell withoutsupervision of an experienced trainer).
Osteocondritis of the spine
Osteochondrosis of the spine is divided into several types. This is:
- Osteochondrosis of the cervical region.
- Osteochondrosis of the thoracic region.
- Lumbar osteochondrosis.
- Osteochondrosis of the sacral region.
Most often, lumbar and sacral osteochondrosis are considered as a single disease - osteochondrosis of the lumbosacral spine. This is due to the structural features of these sections of the back (we will consider this in the relevant sections).
In some cases, osteochondrosis of the coccyx may develop when the articular cartilage between the sacrum (in adults it is 5 fused vertebrae) and the coccyx (it consists of 3-5 vertebrae) is affected. This disease is most common in women after spontaneous childbirth (especially when the mother has a narrow pelvis or the fetus weighs more than 4 kg), but can develop with injuries, operations and malformations of this spine. Due to the structural features of the sacrococcygeal joint (the absence of a nucleus pulposus in it - a central shock-absorbing area that exists between the vertebrae of the cervical, thoracic and lumbar regions), it is more correct to call articular cartilage damage in it arthrosis of the sacrococcygeal joint than osteochondrosis.
Osteochondrosis can also develop in more than one part of the spine. When such a process develops in more than two, it is called widespread.
The symptoms of each type of disease are discussed in detail in the article "Symptoms and signs of osteochondrosis".
A little more about terminology. Scientists (4) believe that the phrase "intervertebral osteochondrosis" is unacceptable. Firstly, as a result of this process, both the vertebral bodies are affected (this is displayed in the prefix "osteo-"), and articular cartilage - the endplates of the vertebral bodies ("-chondrosis"). That is, not only the intervertebral discs suffer, but also the structures surrounding them. Therefore, it will be correct to say "osteochondrosis of the spine", and not in any other way.
Osteochondrosis of the cervical spine
The cervical region is distinguished by the following features:

- this is the only part of the spine where the intervertebral disc is not everywhere between the vertebrae: it is absent between the 1st vertebra and the back of the head, as well as between the 1st and 2nd cervical vertebrae;
- the lateral parts of the underlying vertebrae cover the overlying vertebrae from the sides: it turns out that the latter seem to be sitting in a "saddle";
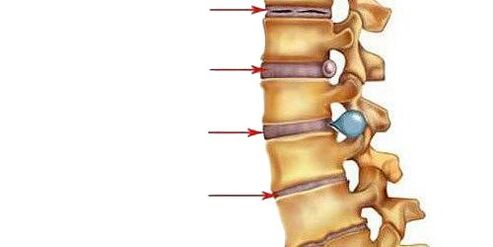
- the edges of the bodies of the cervical vertebrae are elongated and look a bit like a hook pointing upwards, which is why they are called "hook-shaped". Such a "hook" and a section of the overlying vertebra are not just in contact: between them there is the same joint as in the limbs: from above, the articulating surfaces are covered with articular cartilage, and the articular capsule wraps the joint. These joints allow you to perform additional, inherent only in this department of movement - tilt and rotation. But they "carry" additional problems - arthrosis (thinning of the articular cartilage) can develop in them. And this is where osteophytes are formed. This is dangerous: nerve fibers or blood vessels passing in these departments can be squeezed by osteophytes.
With the development of osteochondrosis in the cervical region, when the intervertebral discs become thinner, and the vertebrae themselves seem to sag, nutrition and the joint between the "hook" of the underlying vertebra and the body of the overlying vertebra are disturbed. In this case, arthrosis of this joint becomes a complication of osteochondrosis.
In the cervical vertebral segment, all types of movements are possible:
- extension and flexion;
- side bends;
- turns,
while the volume of these movements is quite large. This is a danger in terms of the development of osteochondrosis, which is characteristic only for the cervical region.
The greatest mobility is observed in the joint between the 4th and 5th, as well as 5th and 6th cervical vertebrae (10, 11). Osteochondrosis does not affect the articular surfaces between the 1st vertebra and the back of the head, as well as the articular cartilage between the 1st and 2nd vertebrae.
The most important structures in the cervical region are:
- on the lateral surfaces of all cervical vertebrae, in their transverse processes, there are openings for the vertebral artery to pass here, carrying blood to the brain;
- inside the first cervical vertebra (it is very different from the "ordinary" cervical vertebrae) there is a transition of the brain stem to the spinal cord;
- below 1 cervical vertebrae, the first cervical roots of the spinal nerves begin to emerge from the spinal cord. Further, between the two vertebrae (upper and lower), one pair of spinal nerves exits (between 1 and 2 vertebrae, 1 pair of nerves exits, between 2 and 3 - the second, and so on). The first three of them go to the neck and its organs (thyroid gland, pharynx, larynx, trachea), partly to the eyes and ears. The fourth pair of spinal nerves goes to the main respiratory muscle - the diaphragm, from the fifth to the seventh pair they innervate (provide nerve signals) to the hands.
With osteochondrosis and its next stage - a hernia of the intervertebral disc, any of these structures can be infringed. These are very life-threatening conditions. But most often, osteochondrosis develops in the lower cervical regions, infringing on either 5, or 6, or 7 spinal nerve roots, due to which sensitivity (tactile, temperature, vibration) and mobility of one of the hands are disturbed, and pain occurs in it (with thatside where the intervertebral foramen narrowed).
Osteochondrosis of the thoracic region

This form of osteochondrosis is quite rare. This is due to the small amount of mobility in the thoracic region.
Each of the thoracic vertebrae is connected not only to the vertebrae (top and bottom), but also to the ribs (each vertebra is connected to a pair of ribs). This ensures the stability of the thoracic region and limits the mobility of the spine.
The openings through which the spinal nerves exit are smaller than in other departments. Already the canal in which the spinal cord passes. Therefore, its even greater narrowing with the growth of osteophytes (bone "thorns" from the vertebrae) may develop a violation of the blood supply to the spinal cord (spinal stroke).
As part of the thoracic roots of the spinal nerves (there are 12 of them, like the vertebrae), a large number of nerves of the autonomic nervous system pass. Therefore, when the nerve fibers in the thoracic region are infringed, then in addition to disrupting the functioning of the organs to which they go:
- from the root between the last cervical and first thoracic vertebrae, part of the nerve fibers goes to the eye (pupil, circular muscles of the eye);
- from the first two segments - to the hands;
- from the second and the remaining ten - to the organs of the chest cavity (heart, lungs, large vessels), to the organs of the abdominal cavity (liver, stomach) and retroperitoneal space (pancreas, kidneys) (1),
There will also be symptoms of disruption of the autonomic nervous system: arrhythmias, anxiety or fear of cardiac arrest, sweating, a feeling of heat (the so-called "hot flashes"), pallor, rapid breathing.
In addition, the fourth segment of the spinal cord, which is located at the level of the 2nd thoracic vertebra, is a critical area of blood supply to this organ. With a decrease in the diameter of the spinal canal, a spinal stroke (death of part of the spinal cord) will develop faster here than with infringement of the spinal cord in other places.
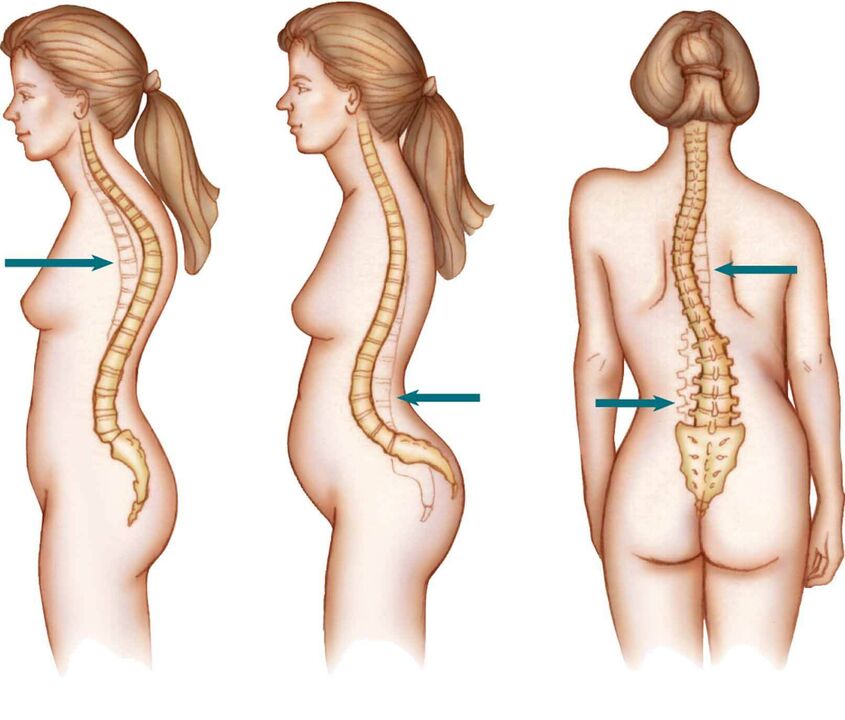
Osteochondrosis rarely develops in the disc between 1 and 2, as well as between 2 and 3 vertebrae. More often it occurs in the region of 6-7 thoracic vertebrae, where there is a maximum backward curvature of the spine (kyphosis).
Osteochondrosis of the lumbar spine

Osteochondrosis of the lumbar spine occurs in approximately 50% of cases. This is due to the large load on this section of the spine (it has to support the weight of the body), which increases even more with squats (muscular work plus a change in the center of gravity of the body), weight lifting, some incorrect movements (for example, when playing football, when you have tocatch the ball, performing muscular work, moving the center of gravity not to the center, but to the edge of the joint between two vertebrae).
In addition, the lumbar region is very mobile and connects the inactive thoracic spine and the immobile sacral.
Most often, the lesion of the intervertebral disc, from which osteochondrosis begins, corresponds to the gap between the 4th and 5th vertebrae (the top of the lumbar lordosis is observed here - the bulge of the spine), less often - between the 5th lumbar and 1 sacral vertebrae. These segments are the most overloaded. The discs between the 1st and 2nd and 2nd and 3rd vertebrae are affected less frequently as they have good mobility.
Osteochondrosis of the sacrum

Isolated osteochondrosis of the sacral region rarely develops. This is due to the fact that the vertebrae are fused here, and the entire load is forced to be distributed immediately to the entire department. Osteochondrosis in the sacrum develops when the lumbar region has suffered (due to osteochondrosis, injury or other disease), and the fused five vertebrae have to withstand the increased load.
In the absence of spinal abnormalities, the sacrum should be at a 30-degree angle to the vertical axis of the body to maintain balance with the tilted pelvic bones. But if the first sacral vertebra protrudes forward a little more than necessary (due to a congenital anomaly or injury), this will limit the space for the roots of the spinal nerves emerging from the 1 sacral segment, as well as the vessels. If this is combined with sacralization (the growth of the last lumbar vertebra to the first sacral), then the places for the roots of the 2nd sacral segment will also be narrowed. Then the osteochondrosis that has developed here (especially posterior osteophytes) and its complications (intervertebral hernia) will quickly make itself felt with a pain syndrome localized in the perineum and inner thighs.
It should be noted that the sacralization of the spine does not occur immediately after birth. The fusion of the last lumbar vertebra with the sacrum begins at the age of 13-14, and ends by the age of 23-25. There are situations when the first sacral vertebra remains unattached all life, performing the function of the 6th lumbar. Such anomalies create more prerequisites for the development of osteochondrosis here, and are also often combined with non-closure (complete or partial) of the sacral canal - a curved tube in which the sacral nerves exit the spine through the sacral foramina.
Osteochondrosis of the cervical and thoracic spine
Osteochondrosis of the cervical and thoracic spine occurs when a person does not pay attention to the developed dystrophic process in the discs between the lower cervical vertebrae. As a result, "circles on the water" begin to diverge from such a "stone" - the underlying (thoracic) spine begins to be involved in the process.
The situation when segments from the cervical and thoracic regions, which lie far from each other, are subject to changes in the disk and the vertebrae surrounding it, develops less frequently.
Osteochondrosis of the lumbar and sacral
The entire sacrum and the last vertebra of the lumbar are the basis of the entire spine - they provide its support and experience the maximum load. If additional loads fall on it, especially if genetic, hormonal prerequisites develop for this, or a person constantly experiences a deficiency of microvibration, osteochondrosis of the lumbosacral region develops (more on this can be found here: "Causes of osteochondrosis").
The discs between the lumbar vertebrae usually suffer first, then (according to the mechanism described in the previous section) the sacrum is involved in the process. Also, lumbosacral osteochondrosis is often called a condition when the joint between the last lumbar vertebra and the sacrum undergoes dystrophic changes.
Widespread or polysegmental

The disease develops in 12% of cases of osteochondrosis. This is the most severe type of disease, when dystrophic processes occur in several segments (a segment is two vertebrae, upper and lower, surrounding the affected intervertebral disc) of the spine. Both segments of one department (for example, osteochondrosis of the disc between the 4th and 5th and 6-7th cervical vertebrae) and unrelated segments of different departments can be affected. For example, osteochondrosis of the disc between 4-5 cervical vertebrae (C4-C5) and the disc between 4 and 5 lumbar vertebrae (L4-L5) may develop.
Since with polysegmental osteochondrosis it does not happen that an exacerbation develops in all departments at the same time. Most often, an exacerbation develops in one department, then in another. This led to the emergence of such a "household" diagnosis as wandering osteochondrosis. Official medicine does not recognize it and appoints a person who has made such a "diagnosis" to himself additional studies in order to understand the cause of his symptoms.
Stages (periods)
Modern literature describes osteochondrosis of the spine as a chronic process prone to recurrence. Developing at a young age (mainly as a result of injuries or improper movements, weight lifting), it progresses at different rates, can slow down (remission of osteochondrosis occurs), or can proceed continuously. In the elderly, on the contrary, a slow course of the disease is observed.
Neurologists distinguish several stages (periods) depending on how the structures of the intervertebral disc are changed:
- I period.Here, there is a decrease in the amount of water in the composition of the nucleus pulposus - the shock-absorbing center of the intervertebral disc, and cracks appear in its fibrous ring. The nucleus pulposus is deformed and shifted posteriorly (towards the posterior longitudinal ligament, which runs along the posterior surface of the vertebral bodies). Such an intradiscal movement of the nucleus pulposus causes irritation of the passing nerves (in the cervical region - sinuvertebral). This is manifested by minor pains in the neck or the corresponding part of the back, stiffness of movements, the adoption of a special posture in which there is some pain relief. If osteochondrosis develops in the lumbar region, the lumbar lordosis is smoothed out.
- II periodcharacterized by the formation of subluxations, pathological mobility in the affected segment of the spine. This is due to the fact that the cartilage-like tissue of the disc (annulus fibrosus), which lies around the nucleus pulposus, begins to gradually dry out - the height of the disc decreases. Where the annulus fibrosus is more stratified, the nucleus pulposus rushes, helping to further deflate it (usually this happens in the direction of the weaker posterior longitudinal ligament). This period of osteochondrosis is manifested by pain at the level of the affected segment, the muscles above and below the segment are constantly tense, trying to hold the vertebrae so as not to damage the spinal cord.
- III periodcharacterized by a complete rupture of the fibrous ring, so the nucleus pulposus makes a move in it and protrudes between the vertebrae (an intervertebral hernia is formed). The nucleus pulposus may even prolapse into the lumen of the spinal canal (disc sequestration). The cartilage covering the vertebrae is thinning due to the fact that the layer between them becomes smaller. The symptoms of the stage depend on the direction in which the intervertebral disc is displaced: if in the direction of the opening through which the spinal root exits, pains will be felt that spread along the nerve fibers (that is, if osteochondrosis develops in the lower cervical or upper thoracic segments, theywill be felt in the arm, and if in the lumbar - then in the leg), the sensitivity of the innervated organs suffers; if in the direction of the spinal canal along the midline, the back pain becomes constant, the mobility and sensitivity of the limbs are disturbed, the function of the internal organs that receive innervation from the affected segment suffers, if the nucleus pulposus penetrates into the vertebra located above or below, there will be an asymptomatic course of the disease;
- IV period.The tissues of the affected intervertebral discs are replaced by scar tissue, due to which mobility in this spinal segment is limited or lost. In neighboring segments, the vertebrae are forced to shift, inflammation and arthrosis develop between their processes. Osteophytes begin to appear from the bones - bone outgrowths. The longitudinal ligament may ossify. The edges of the vertebrae deformed by osteophytes and the ossified ligaments next to them form a kind of bone brackets. This is spondylarthrosis.
When muscles are involved in the process, trying to stabilize the spine, a spasm occurs in them, local vessels are squeezed. Because of this, edema develops, which compresses the nerve roots. There is pain. This is -spicyperiod of illness. If you start treatment in this period - limit motor activity in the damaged section, use painkillers (they are also anti-inflammatory) drugs, thenattackosteochondrosis disappears in 5-7 days. Subacute or2 perioddiseases.
The subacute period lasts approximately 12-14 days. If at this stage you do not overcool, do not lift weights, do not make sudden movements, osteochondrosis goes into remission.
Aggravationosteochondrosis rarely develops "on its own" if a person takes care of replenishing the microvibration deficiency in the body (this is achieved with the help of high motor activity and/or phonation procedures) and maintaining sufficient blood supply to the affected area.
Exacerbation of osteochondrosis can cause:
- hypothermia;
- weight lifting;
- severe stress;
- abrupt movements;
- unprofessionally performed massage;
- alcohol intake;
- cold;
- a sharp change in heat and cold (for example, diving into cold water after a bath or sauna);
- frequent bends;
- long stay in a bent position.
Degrees of osteochondrosis
In its development, osteochondrosis goes through certain stages. They are called degrees, and depending on the degree, the doctor plans treatment.
To understand how the disease affects work, the ability to self-service, the adequacy of a person, domestic neurologists distinguish 5 degrees of osteochondrosis:
Degree |
Severity of pain and other symptoms |
Violation of working capacity and working capacity |
|---|---|---|
1 degree |
At the first degree, the pain is insignificant, occurs during exertion, and disappears at rest. Only pain points can be detected. |
Saved when doing any work |
2 degree |
The pain is not severe, it appears at rest, it increases with exercise, but if you take a comfortable position or stop the exercise, the pain disappears. In the second degree, a change in the configuration of the spine is noticeable, tense muscles are felt. Limited mobility of the spine |
If we are talking about a worker of non-physical or light physical labor, working capacity is preserved. If a person works hard, the ability to work is limited. A person is forced to pause at work, tries to avoid physical exertion |
3 degree |
The pain is more pronounced, aggravated by exertion. Neurological symptoms that violate the ability to work are revealed. |
Violated. Only knowledge workers can continue to work. The ability to perform household activities is reduced, but self-care and the ability to move independently are preserved |
4 degree |
In addition to severe pain, neurological symptoms also appear: dizziness, impaired sensitivity |
Lost for any work. Can move within the premises, only leaning on crutches. He tries to move only when it is necessary to satisfy physiological needs. |
5 degree |
Pain and other symptoms are pronounced at rest. The person is forced to stay in bed. |
Lost for any kind of work. The person needs care. |
Osteochondrosis of the spine, in whatever department it is formed and whatever degree it has reached, needs to be identified and adequately timely treated. At the same time, treatment should be comprehensive, and include not only taking medications to relieve symptoms, but also other (main) methods of treatment aimed at eliminating the causes of the disease.
















































